FHIR - An Incremental and RESTful Approach to Health Data Interoperability

Introduction:
HL7 International is the company behind the Fast Healthcare Interoperability Resource, a draft data standard. In order to connect several separate pieces, FHIR uses a cutting-edge, internet-based methodology that was designed with the complexity of healthcare data in mind.
The goal of FHIR is to create a foundational set of resources that, individually or in combination, may be used to address most typical use cases. The fundamental information set that is shared by the majority of implementations is the focus of FHIR resources "According to HL7's website.
Similar to the URL of a web page, each piece of data, or "resource," has a tag that serves as a special identification number.
Fast Healthdata Interoperability Resource, or FHIR for short, is a data standard created and supported by HL7 International that uses the internet to link various health systems.
No matter what EHR "operating system" the user's infrastructure uses to access data, FHIR enables the development of standardised "browser" apps.
Due to the disparate data models utilised by the systems, it is frequently challenging to reconcile health information amongst healthcare IT systems. This is viewed as an expensive and time-consuming task. By providing an open interoperability standard that is compatible with the most recent web standards and based on service-oriented architecture, FHIR tackles this problem.
What makes FHIR different from other health interoperability standards:
The majority of health information interchange today is document-based, which makes it difficult to effectively coordinate treatment, make decisions, or analyse data. It also takes extra work to gather the data from standards like C-CDA and make it useable in other formats, despite the fact that they contain a lot of crucial information. Additionally, document-based information transmission is finished, but it prevents a provider from exploring the context of the data they have received. When the user is missing the patient's history, simply delivering lab results or a list of allergies is insufficient.
Although the patient-generated health data (PGHD) flowing from millions of FitBits, Apple Watches, Bluetooth scales, blood glucose monitors, diet applications, and fitness trackers integrated into provider workflows is rising, no technology has been able to connect it as of yet. Such a pool of PGHD is useless if the providers cannot rapidly and readily access it. Users will be able to undertake various downstream operations like data analytics and display patterns important to aspects of say, chronic disease management or patient wellness, thanks to the ability to access this PGHD that would otherwise be "locked" by FHIR on an FHIR platform.
In the healthcare sector, the FHIR protocol is currently widely utilised in server communications, cloud communications, EHR-based data sharing, and mobile applications.
Components of FHIR standard specification:
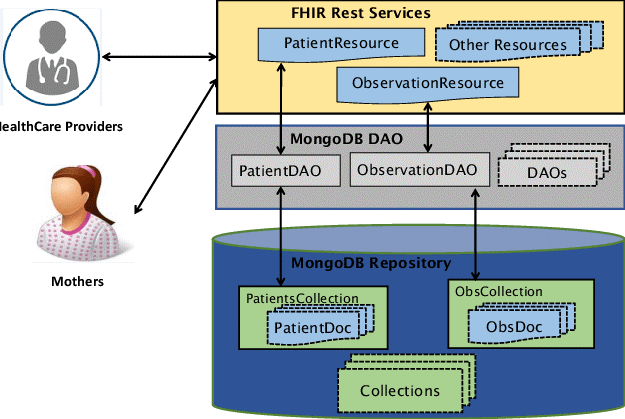
The primary objective of FHIR is to offer a basic set of data pieces known as resources, which, when coupled via references, should cover the majority of clinical use cases. The augmentation mechanism known as profiling supports additional scenarios that emerge in particular health areas. The three key facets of FHIR development are resources, references, and profiles. Let's go over each one.
In the health sector, the FHIR standard is currently widely utilised in server communications, cloud communications, EHR-based data sharing, and mobile apps.
- FHIR Resources: Resources are the primary structural component of FHIR solutions. Resources are data exchange or storage packets that cover the majority of use cases in the therapeutic setting. For instance, a source About a person or animal getting care, the term "patient" refers to administrative and demographic information. Numerous resources exist that cover several facets of the healthcare industry, including scheduling, patient administration, medical billing, and information tracking. Resources specify what data will be communicated through them and can be represented in a variety of forms (UML, XML, JSON). They may also include plain text that includes explanations.
- FHIR Reference: Rarely are resources used separately, and the majority of them have references to other resources. You can implement and customise particular situations by connecting Patient to Observation (which saves statements made about a patient), Condition (problem or diagnosis), and Medication (ingredients, amount, and strength of medications). References can be given in the form of a text description, an explicit identification, or a URL.
- FHIR Profile: A resource's utilisation in a given situation is specified by a profile. Developers publish their adaptations in Implementation Guides, another FHIR Healthcare standard, and explain how their FHIR-based APIs might be used there.
One of the most difficult FHIR implementation tasks is profiling: It necessitates a thorough knowledge of all FHIR resources as well as the technical details of implementation. Consequently, to promote interoperability, Consequently, a tool with built-in profiles was developed to aid with interoperability.
FHIR's architectural Principles:
Reuse and Composability, Performance, Usability, Data integrity, Scalability, and Implementability are the six architectural concepts that make up FHIR. The first four principles are related to the data structure, scalability and the exchange mechanism are related, and structure and data exchange are both related to implementability.
Maturity stages of FHIR Resources:
The life cycle of FHIR Resources includes the following stages, with "Normative" being the most stable of them all:
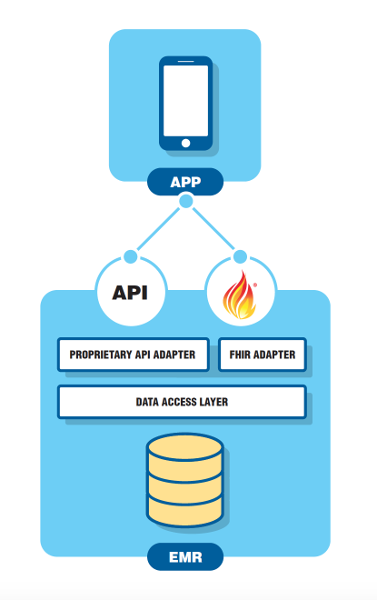
FHIR API:
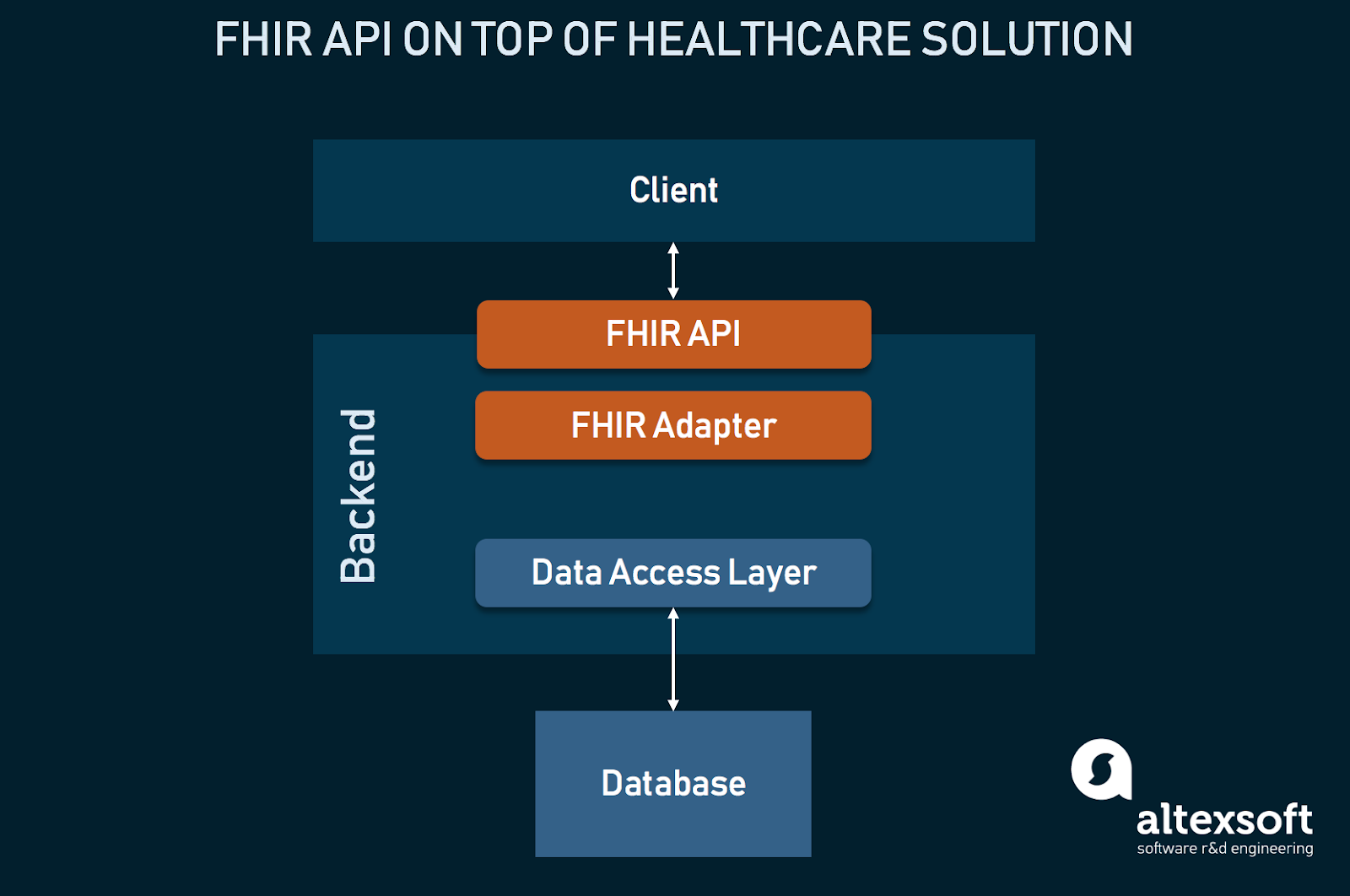
Based on known web standards, FHIR offers specifications for an Application Programming Interface, or API. APIs are widely used in contemporary desktop and mobile applications for retrieving, storing, and updating data. An API is a point of entry, or "interface," via which another piece of software can access the functions and information of another piece of software.
Understanding REST Architecture:
REST (Representational State Transfer), an information exchange standard, serves as the foundation for many web and mobile applications' APIs. The World Wide Web standard transmission protocol HTTP, the fundamental internet standard that serves as the foundation for all website data exchange, is a technique of information interchange known as REST.
REST is made up of a client request and a server response. A "RESTful" exchange is one where REST is used to share data. RESTful designs provide the benefit of minimalist interfaces that enable quick data transfer and processing, making them suitable for mobile and tablet devices.
In its API, FHIR bases data sharing on the REST architecture. A RESTful HTTP command is used to ask the servers for the interoperable data components within FHIR known as Resources. Servers are built with the kinds of Resources and interactions they can support, like those powering an electronic medical records system.
FHIR uses the REST architectural style to establish an up-to-date approach of interoperability by combining the greatest features of current health information technology and widely used internet standards. This enables speedier application design and enables health care systems to use FHIR with less challenging learning curves.
Knowledge of FHIR Server:
A FHIR server is described as having the following capabilities:
- Accept a request from a RESTful API
- Read the RESTful API request carefully
- Implement the request
- Please respond
At the very least, the FHIR Server is supposed to return a Capacity Statement outlining its capabilities.
The messages delivered must be self-descriptive because no previous FHIR messages are saved on the server.
Resources are shown in formats that the client and server can comprehend, such as JSON and XML.
Both the server and the client should be able to comprehend how the resource identity (URI) is expressed.
The FHIR Request to Server: Understanding
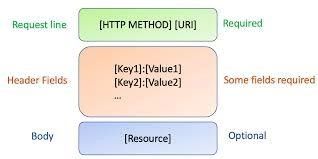
There are three parts to an FHIR Request that the server receives:
- Request line: Consists of the [URI] and [HTTP method]. The Request structure requires that this be done.
- The HTTP method directs the server's actions.
- For Uniform Resource Identity, use URI. The required Resource is indicated by a URI. The resource type, such as Patient Resource, is specified by the resource identification.
- field headers: Key-value pairs [key1]: [value1] make up these. some of which might be necessary.
- Body: Made up of a Resource. Within the request structure, it is optional.
Understanding the Server's FHIR Response
Three parts make up an FHIR response:
- Status Line: This describes the interaction's status and includes the [status code] and [Reason]. It is necessary for the response's structure. It includes details like Success/Failure.
- Headers Fields: Similar to the request Header fields, they are key value pairs with the format [key1]: [value1]. some of which might be necessary.
- Body: Made up of a Resource. It's not required.
FHIR API Interactions
The following list of FHIR interactions is the most typical:
FHIR API Integration is a position to serve as the fundamental "network" connecting various health services. In a secure healthcare ecosystem where patients can easily access their data and clinicians can quickly and easily access data from external systems, FHIR will continue to promote the interoperability of health information, providing providers and patients with access to a remarkably rich set of functionalities. FHIR is positioned to be the future of global healthcare interoperability due to its simplicity of use and mass acceptance as a result of its connection with the internet.
Conclusion: The HL7 DaVinci Project, which has assisted payers and suppliers in improving clinical reliability, price, and patient care outcomes, and the Argonaut Project, which assisted users of a top platform aggregate and access personal health data on their mobile devices, are two examples of the success the FHIR community has experienced over the past ten years. FHIR holds a lot of promise, and the data standard is well-supported throughout the entire care continuum. According to James Agnew, chief technology officer at Smile CDR and an early adopter of FHIR, "FHIR is poised to become the underlying 'network' that underpins health applications worldwide."
According to study results from the Engine Group conducted in April 2021 under contract with Change Healthcare, just 24% of healthcare organisations currently use FHIR APIs at scale, but 67% of providers and 61% of payers anticipate their organisations using APIs at scale by 2023. Providers and patients will have access to an exceptionally comprehensive set of functions within their health IT systems as long as FHIR remains the foundation for data sharing.