HEDIS Measures - Why Should We Care?
Introduction:
Value-based healthcare has encouraged a mindset of steady improvement in the delivery of clinical outcomes, with the ultimate goal of increasing outcomes without introducing extra or needless expenditures. Most consumers have this objective in mind when selecting a health plan.
One of the most popular healthcare performance measurement tools, the Healthcare Effectiveness Data and Information Set (HEDIS), is used by the majority of health plans to assess their quality and performance. In order to compare health plan performance and assist consumers in choosing the best healthcare coverage, HEDIS offers a set of measurement standards.
HEDIS BENEFITS:
Health care plans can better understand the quality of care given to its members in the most prevalent chronic and acute illness populations by using the results of the metrics. Other advantages of HEDIS include:
- Allows for the discovery of shortcomings in the performance of the healthcare network and the delivery of services
- Uses preventative services to enhance patient outcomes and lower healthcare costs.
- Data about public health problems that affect large patient populations, such as cancer, heart disease, smoking, asthma, and diabetes, may be useful.
- Providers may be able to track the success of quality improvement activities by using measure patterns.
HEDIS' Objectives:
The National Committee for Quality Assurance (NCQA) developed the quality measures that make up HEDIS. The performance of health plans is tracked yearly using this data, which also offers useful details about the patient populations treated. The metrics monitor the actual care provided, not just what was prescribed. The information gathered is used to spot areas that could use improvement and to:
- Keep track of people's general health.
- Analyse patient treatment methods and results.
- Offer a third-party performance measurement.
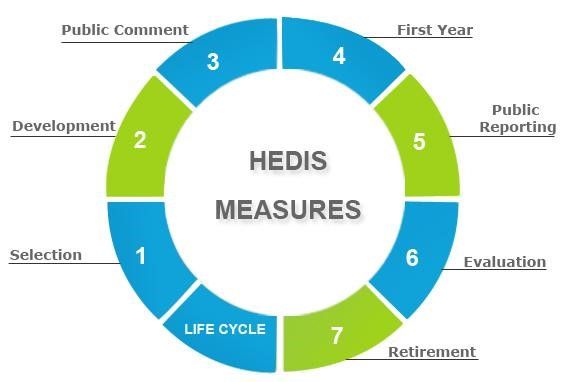
Since certain HEDIS measures are retired and new ones are added, the number of HEDIS measures changes every year. Aspects of healthcare are covered by the measures, including preventative care such as vaccines and screenings, management of physical and mental health disorders, access to care and availability, patient experience, healthcare use, and resource use.
For the purpose of evaluating the standard of preventive care offered by health plans, the first set of HEDIS assessments was created in 1989. Since then, other measures have been added in an effort to evaluate various care settings and gradually raise the standard of healthcare. More than 200 different measures have currently been included in the program. The following is a list of some of the most typical ones:
HEDIS Measures:
- Treatment's effectiveness
- Treatment is available and accessible.
- Having quality care
- Utilization as well as Risk-Adjusted Utilization
- Descriptive data regarding the health plan.
- Amounts Reported by Electronic Clinical Data Systems.
- Access to Care: Covers the proportion of plan participants who are qualified to receive healthcare as well as the extent of their coverage for each service. Preventive services like immunizations and cancer screenings are included, as are fundamental medical services like dental services and prescription drug coverage.
- Clinical Quality: assesses the quality of patient care given in accordance with guidelines established by the medical community. Examples include assessments of patient satisfaction, the frequency of problems following surgery, and the proportion of patients who leave a facility within the advised time period.
- Financial Coverage: Calculates the costs of providing care to plan participants. These include the cost of premiums or co-insurance as well as out-of-pocket expenses like co-payments and deductibles.
- Services for health care: Evaluates the range of services a plan offers its members, as well as their standard and accessibility. This can include the availability of doctors, hospitals, and pharmacies as well as the services each facility offers. There are lot of Healthcare Integration Services for better results.
- Healthcare Plan Customer Quality: Evaluates how satisfied plan members are overall with the services their medical insurance provides. This includes evaluations of the level of care delivered, the simplicity of accessing services, and the plan's level of customer service.

Collectively, these metrics aid in highlighting areas where plans are succeeding and those that might use improvement to give their members the best care possible. In order to determine which plans, offer the highest level of care at the most reasonable cost, they also serve as a basis for comparing various plans against one another. There has been a lot of discussion in recent years regarding the various measurement methods and how they are utilized to decide what plans and services to offer.




